Apart from the known and recognized forms of diabetes, there is also a much rarer type of Diabetes Mellitus which affects infants and new born children and is known as Congenital Diabetes. This disorder is also referred to as Neonatal Pseudodiabetes Mellitus as it exhibits slight differences in clinical nature from the more common forms of diabetes. In most cases, Congenital Diabetes proves to be fatal and is considered to be a serious condition.Manuels d’utilisation.

This condition is extremely rare and there are only very few reported cases of Congenital Diabetes [1]. As such, not much is known about the pathogenesis of the disease, and the cause of the condition is completely unknown. In fact, Congenital Diabetes is considered to be a controversial subject, with many medical experts dismissing the condition as a form of diabetes given the significantly lower occurrence rates and some others considering the disease to be related in some way to Diabetes Mellitus as some of the aspects of the condition completely comply with those of diabetes.
Conditions of Congenital Diabetes can only be found in infants between six months to twelve months of age. If undiagnosed, the disease may prove to kill the infant. However, in some cases, the infant may survive and this may lead to many other complications later in life.
When diabetes in diagnosed in an infant, it is a must to be able to correctly determine whether it is a case of Type I Diabetes or a case of Congenital Diabetes. Often misdiagnosed as Type I Diabetes, the treatment is commenced in infants and this helps control the blood glucose levels. However in such cases, there are development delays exhibited by such sufferers in various aspects of life.
If diagnosed properly, all of the complications as well as the conditions of Congenital Diabetes can be controlled. This may be done either with the help of external administration of insulin, or through the use of some specific medications. Early diagnosis can also help distinguish between the different types of Congenital Diabetes and this in turn can help with offering a prognosis and in defining the future lifestyle choices, diet conditions and medication to be followed in order to prevent recurrences or in order to successfully manage conditions of recurrence of the disorder.
Congenital Diabetes can affect infants even before they reach six months of age in some special cases and as such, any infant below one year of age, who is exhibiting signs and symptoms of diabetes such as that of hyperglycemia, can be suspected to be affected by Congenital Diabetes.
Any form of diabetes in which the sugar levels of the blood are higher than normal should be considered seriously. There can be a number of nasty and serious complications associated with diabetes and with conditions of hyperglycemia and these must be avoided at all costs and measures.
Neonatal Pseudodiabetes Mellitus
This form of diabetes is very rare and is often not even included under the different categories of diabetes as it exhibits certain differences from the other clinical signs and symptoms of diabetes. Typically, the disorder is found in infants and new born children below six months of age.
Congenital Diabetes is considered to be different from Type I Diabetes as it does not involve any destruction of the insulin producing cells of the body present in the beta cells of the pancreas and is not considered to be an autoimmune disorder. Type I Diabetes is also diagnosed in children who are above six months of age and this is also one of the major differences between Type I Diabetes and Congenital Diabetes.
Congenital Diabetes is considered to be caused due to changes having occurred to the genes of the infant, which in turn produce a decrease in the production rate of the insulin hormone in the body. Consequently, the sugar level in the blood rises much higher than normal and this is why some medical experts argue that Congenital Diabetes should be classified under Diabetes Mellitus, even though it may be a much rarer and significantly less reported condition.
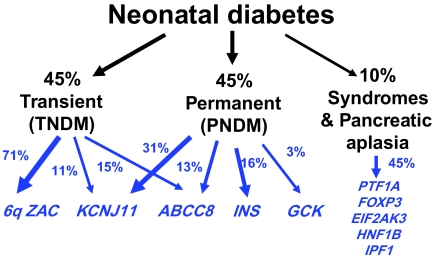
As per the reported conditions, it is believed that a change caused to the either the KCNJ11 or the ABCC8 genes can lead to a development of Neonatal Pseudodiabetes Mellitus. The condition is also considered to be associated with the maternal pedigree and many have reported unexplained cases of infant deaths on the maternal side, which are largely suspected to have been caused due to complications resulting from Congenital Diabetes. However, the occurrence of the disease in very rare and there are only a handful of reported cases all over the world and this makes it extremely difficult to be able to determine the exact cause of the disease.
Signs and Symptoms of Congenital Diabetes
The most important and vital sign of Congenital Diabetes is a high concentration of serum antibodies of insulin and glutamic acid decarboxylase in the blood stream. This results in a lower concentration of insulin as well as the C-Peptide serum in the body. Even through the external administration of either glucose or glucagon the C-peptide serum levels remain close to indiscernible.
This reduction results in a steady buildup in the concentration of the blood sugar levels and many of the vital organs of the body such as the heart, the lungs, as well as the pancreas are targeted by lymphocytic infiltration conditions.
Lymphocytic infiltration results in a larger than normal concentration of T Lymphocytes in the blood, most of which are activated T-Cells. A consequence of this high concentration of T-Cells results in a higher concentration of the serums IgA and IgE in the blood stream.
There are no other reported abnormalities of the functioning of the immunologic system. It is however believed that genetic features, primarily from the maternal side are somehow related to development of this extremely rare condition.
Sufferers of Congenital Diabetes may also exhibit various other symptoms including episodes of vomiting and nausea, diarrhea and problems with digestion and sudden and drastic loss in body weight.
There may also be some delays in the normal development of an infant as a result of Congenital Diabetes. Some of the observed developmental delays exhibited by such infants include the following;
- Clumsy walking or being very slow in walking
- Talking slowly and finding difficulty in learning how to talk
- Difficulty with concentration
- Epileptic episodes may also be experienced in the first year of life of the infant
- Difficulty in social situations
- Difficulty in understanding numeracy or math
Diagnosis of Congenital Diabetes
Typically, there is no complication associated with pregnancy in cases of Neonatal Pseudodiabetes mellitus [4]. In fact, Congenital Diabetes can be diagnosed in infants through the process of genetic testing for any infants around six months of age. A blood sample is used for this diagnostic procedure and is examined in a medical laboratory to check for abnormalities in the blood serum IgA and IgE concentrations, insulin levels and a high concentration of T-lymphocytes. Glucose concentration in the blood stream is much higher than normal levels and ketoacidosis is also occasionally observed.
Genetic testing of a blood sample can help in improving the clinical management as also in predicting the prognosis of the condition. Mutation of genes in the K-ATP channels of the pancreas is usually tested for in the blood sample. In some cases, these genetic mutations occur on their own in an individual. The individual may also prove to have a diabetic relative, with a pattern of autosomal dominant inheritance and the transmission of the defected gene from generation to generation.
Some medical centers offer free testing for the condition. However, a diagnosis of the condition is confirmed only after proper molecular genetic testing has been carried out on the blood sample of the infant.
In case you suspect that your infant may be suffering from Congenital Diabetes conditions and is under the age of six months, genetic testing should be carried out at the earliest in order to diagnose the condition and also to be able to effectively control the disorder.
Complications associated with Congenital Diabetes
Congenital Diabetes can prove to be a serious and life threatening condition if it is not diagnosed and provided with proper treatment at the right time [3]. While conditions of hypoglycemia, fatigue, weakness and less resistance to infection are commonly exhibited, the loss of weight and an inability to show proper development can all lead to serious conditions, often leading to a death of the child below even twelve months of age.
There have been many cases of deaths of infants due to unknown causes and it is suspected that the genetic susceptibility of individuals to encounter the disorder are higher if there have been such cases in the family, typically on the maternal side.
Even after having been successfully treated in infancy, symptoms of Congenital Diabetes may re-manifest during the teenage years of an individual. At such a stage, the complications associated with the condition can prove to be just as severe as that of other types of diabetes and may cause damage to many of the vital organs of the body due to excessive hyperglycemic conditions. If somehow the sufferer is unaware of having the condition, administration of glucagon or other measures may not prove to be effective immediately and may further cause delays in providing treatment processes.
Treatment of Congenital Diabetes
It is estimated that about half the cases of individuals diagnosed with Congenital Diabetes need not be given insulin administration as a necessity [2]. The insulin producing cells are still active in the body and what needs to be controlled is the presence of the insulin antibody serum in high concentration in the blood stream.

Sulphonylurea drugs are also used in cases of Permanent Congenital Diabetes and also Type II Diabetes. One of the most popular forms of this type of medication known as Glibenclamide can be given to the suffering infants in order to control both of the conditions. The medication is also often administered to Type II Diabetes sufferers; however the dosage is typically much higher in the case of Congenital Diabetes. When administered at higher dosages, the medication can prove to stimulate the pancreas to produce and release insulin directly into the blood stream whenever food is consumed by an individual.
Sulphonylurea drugs can help in both controlling the glucose levels in the blood and in improving other associated symptoms of development delay in infants. In many cases, sufferers of Congenital Diabetes are shifted from insulin administration therapy to completely sulphonylurea drug supported medication. Typically, the development delays can be avoided with higher dosages of sulphonylureas
In some of the other cases, both insulin administration and Glibenclamide are prescribed as medication procedures in order to control the condition of Congenital Diabetes. However, such cases are rarer and insulin administration is more often associated with Type I Diabetes treatment.
It is always recommended to obtain recommendation from a licensed medical professional post the diagnosis of Neonatal Pseudodiabetes Mellitus before the administration of any type of medication or resorting to any alternative remedies for treatment.
Plenty of fluids are also recommended to be given to infants suffering from the condition often to be boosted with electrolytes. This can help with dehydration and in controlling other symptoms that are associated with Neonatal Pseudodiabetes Mellitus.
Prognosis of Congenital Diabetes
Congenital Diabetes can be considered to be of two types:
- Transient Congenital Diabetes: This condition, as the name suggests, is only a temporary condition and is usually resolved after the infant reaches 12 months of age. However, symptoms of the disease may recur later on during the teenage years of the individual. It is more common than Permanent Congenital Diabetes.
- Permanent Congenital Diabetes: This condition is a permanent condition and suffers exhibit the signs and symptoms of the disease throughout the course of their lives.
Both of these types of Congenital Diabetes can be controlled with medication. However, as with other forms of diabetes, any individual who has been diagnosed with the condition will have to maintain utmost care in terms of diet and lifestyle in order to prevent any complications that diabetes may have to offer.
References
[1] Risks For All-Cause Mortality, Cardiovascular Disease, And Diabetes Associated With The Metabolic Syndrome, Earl S. Ford, MD, MPH; 28no. 7 1769-1778 – July 2005 – DOI: 10.2337/Diacare.28.7.1769, http://Care.Diabetesjournals.Org/Content/28/7/1769.Short
[2] The Effectiveness Of Disease And Case Management For People With Diabetes, Susan L Norris, Phyllis J Nichols, Carl J Caspersen, Russell E Glasgow, Michael M Engelgau, Leonard Jack Jr, George Isham, Susan R Snyder, Vilma G Carande-Kulis, Sanford Garfield, Peter Briss, David Mcculloch,; Volume 22, Issue 4, Supplement1 Pages 15-38 – May 2002 – DOI: 1016/S0749-3797(02)00423-3, http://www.sciencedirect.com/science/article/pii/S0749379702004233
[3] Vascular Complications Of Diabetes, Richard Donnelly,Alistair M Emslie-Smith, Iain D Gardner, And Andrew D Morris; 320(7241): 1062–1066 – April 2000 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1117946/
[4] Neonatal–Onset Multisystem Inflammatory Disease Responsive To Interleukin-1β Inhibition, Raphaela Goldbach-Mansky, M.D., Natalie J. Dailey, M.D., Scott W. Canna,; 355:581-592 – August 10, 2006 – DOI: 10.1056/Nejmoa055137, http://www.nejm.org/doi/full/10.1056/nejmoa055137
[5] Projection Of Diabetes Burden Through 2050, James P. Boyle, Amanda A. Honeycutt, K.M. Venkat Narayan, Thomas J. Hoerger, Linda S. Geiss, 24 No. 11 1936-1940 – November 2001 – DOI: 10.2337/Diacare.24.11.1936Diabetes, http://care.diabetesjournals.org/content/24/11/1936.short
